This is a sponsored story, created and edited exclusively by Tokyo Metropolitan Government’s Tokyo Updates website.
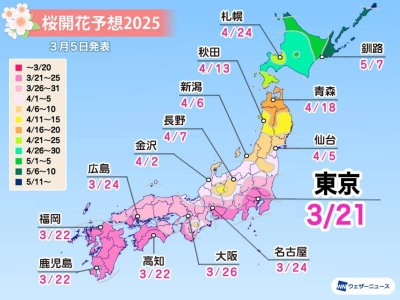
Among Japan's challenges as a super-aging society is a rise in cases of dementia, a disease wherein damaged or ill-functioning brain cells result in reduced cognition that can hinder daily life activities. Approximately 15% of Japan's elderly population (those aged 65 and above) are said to be affected by this condition, with the number of patients in Tokyo alone projected to reach around 540,000 by 2025.
Raising awareness for dementia
The Tokyo Metropolitan Government (TMG) has taken numerous proactive steps to address the issue of dementia, including the launch of its Tokyo Dementia Navi website, which serves as an informational clearinghouse. The Bureau of Social Welfare further held a Tokyo Dementia Symposium on Sept. 17, 2024, in commemoration of World Alzheimer's Day on Sept. 21.
The day's program featured discussions held by specialists in the field, as well as lunch served courtesy of the Restaurant of Mistaken Orders, whose team comprises persons living with the condition.
Dementia across cultures
The symposium's panel of Japan-based experts was joined by Dr. Katarina Nagga, a professor of geriatric medicine at Sweden's Linkoping University. A long-time clinical doctor and researcher in the dementia-related field, Nagga is also a founding member of a Swedish program launched in 2010 to address the challenges of BPSD (Behavioral and Psychological Symptoms of Dementia). The team launched a framework to improve patient care and ultimately reduce these symptoms.
When people with dementia are unable to communicate their needs, Nagga explained, they may develop symptoms of irritability, anxiety or agitation as a means of self-expression. The BPSD approach implements assessments to identify these needs. One example is that it can be difficult to detect the presence of physical pain if the individual cannot communicate it verbally. In such cases, the program encourages the use of a non-communication-based assessment scale, which can help detect the presence of pain by identifying specific facial expressions or body movements.
The BPSD program was subsequently implemented in Japan, and the symposium provided an opportunity for the Swedish and Japanese BPSD research teams to re-touch base with each other's work.
Nagga praised TMG's efforts to increase information and awareness among citizens about the condition, noting that dementia remains both underdiagnosed and undertreated worldwide.
In adapting the Swedish BPSD model for use in Japan, Nagga found that people with dementia in both countries share many common needs. Early detection is crucial, she stressed, because older individuals living alone are less likely to recognize the early symptoms of the disease and seek diagnosis or treatment. In Sweden, many people with severe dementia are admitted to care institutions, while in Japan, home-based care is more common. Nagga strongly supports the development of care programs that help individuals living with dementia receive appropriate care at home.
Looking beyond the medical model
Dementia treatment, Nagga remarks, should not be limited to medical interventions. Instead, she argues that other approaches—such as making adjustments to the living environment and focusing on communication-related needs—should be considered for addressing behavioral and psychological symptoms.
"Pharmaceutical treatments may be reduced through other interventions such as physiotherapy or incorporating more physical movement into one's daily activities to maintain the ability to participate in everyday household activities," she observed, adding that it is important to discuss available options with the person and their family members at an early stage of the condition to ensure that their wishes are respected.
The BPSD program should at all times be based on a scientific, evidence-based approach, Nagga said, highlighting the necessity of working in teams, which might comprise nurses, doctors, and physical/occupational therapists, wherein everyone is on board together to look at the patient from different perspectives while working toward the same person-centered objectives for treatment.
Front-line care workers are key players
Joining Nagga as a symposium panelist was Dr. Miharu Nakanishi, an Associate Professor at the Tohoku University Graduate School of Medicine, who noted that the main players for addressing dementia in Japan are care workers.
"Those caring for persons with dementia often face isolation and loneliness," Nakanishi noted. "It is important for them to know that they are not alone since the same challenges are being faced in other countries too. This can be very encouraging for them."
"Sweden's BPSD model can give Japan's care workers the confidence necessary to employ non-medical, non-pharmacological strategies for dementia-related care," she added.
Her colleague Dr. Atsushi Nishida, visiting professor at the University of Tokyo and director of the Tokyo Metropolitan Institute of Medical Science's Research Center for Social Science & Medicine, also noted that in the past, people with dementia in Japan and elsewhere who expressed symptoms were often given antipsychotic medications, which increased the risk for cardiovascular disease and early mortality.
"At that time, only the symptoms were being considered, but today, we understand that the root causes of such symptoms were actually unmet needs," he added, echoing Nagga. "We must aim to meet these needs through non-medical strategies, which requires a change in perspective."
"Age is the biggest risk factor for dementia, and if the condition is not addressed before it has progressed to an advanced stage, it becomes very difficult to treat—and is sometimes too late," Nagga reiterated.
'You do not have to give up'
Prior to the start of the symposium, a group of TMG officials sat down for lunch in the building's 32nd-floor cafeteria.
Scurrying around the room, taking and delivering orders, were servers with the Restaurant of Mistaken Orders, a program for people living with dementia. Whenever the servers appeared confused, a team of supporters was on hand to help direct them toward the correct table or offer words of encouragement.
The program's philosophy is that food orders may or may not be delivered correctly, and it aims to cultivate an atmosphere of friendliness wherein such errors are met with understanding and simply laughed off.
"Too often, people living with the condition just want to give up, and I wanted them to know that this is not necessary," explains program director Yukio Wada.
He notes that it is of course a faster and more efficient process for meals to be prepared, but that by putting those with dementia in charge of the task, they can feel more in control of their own lives.
The restaurant's logo is a mouth with its tongue sticking out, which Wada explains is a globally recognized facial expression that is often seen after someone makes a mistake — perfectly encapsulating the program's lighthearted ethos.
"I believe that dementia should be approached from the perspective of human rights rather than the matter of providing care," Wada observes. "It is our mission to help create a society where all people can live with human dignity up until the end of their lives."






















With your current subscription plan you can comment on stories. However, before writing your first comment, please create a display name in the Profile section of your subscriber account page.